Neurodegenerative diseases are commonly described as progressive and irreversible. An example of this is Parkinson’s disease. In spite of improved pharmacological options for symptom management, the current treatment has not been able to reverse or even stop the progression of this disease. This has made an early diagnosis essential to increase the probability of better results in patient management.
Table of Contents
Parkinson’s Disease Symptoms
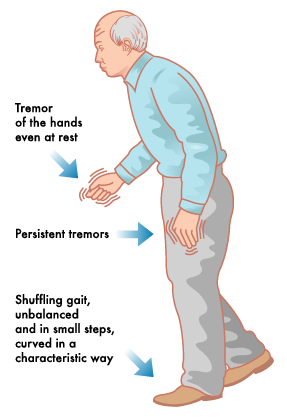
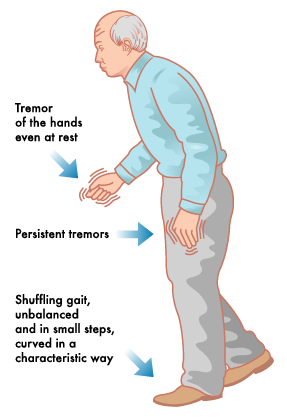
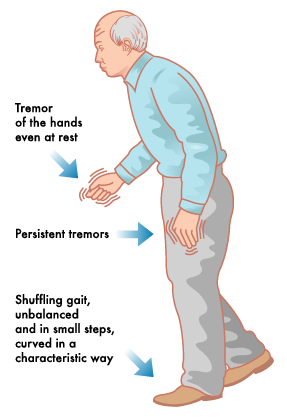
Parkinsons Symptoms
Early signs and symptoms of Parkinson’s disease are subtle, can be confused with other diseases, and are still not completely understood. Early diagnosis of Parkinson’s disease requires proper comprehension of the disease and the clinical experience of the patient. Items that are helpful in diagnosis are the timing of the histopathological changes in the brain, the patient’s risk factors, and signs and symptoms.
Histopathological Changes in the Brain
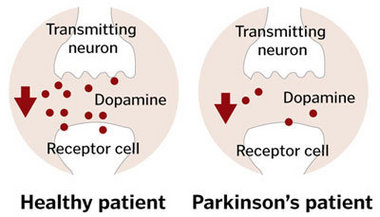
Small, microscopic changes in the brain are the basis of the signs and symptoms of Parkinson’s disease. The typical histological change in Parkinson’s disease on a macroscopic level is the depigmentation of the substantia nigra and the locus coeruleus, which are two small areas in the brain. This change is related to neuron cell death, which is accompanied by the accumulation of protein intracellular inclusions called “Lewy bodies”.
Neurodegeneration is not exclusive to the previously mentioned regions. Other regions affected by neurodegeneration include the olfactory bulb, substantia nigra, raphe nuclei, dorsal nucleus of the vagus nerve, and cortical areas.
The site of these changes can have a direct association with the signs and symptoms of Parkinson’s disease. This is especially true of the substantia nigra, whose function is associated with the control of movement. Changes in the substantia nigra help to explain the major signs of Parkinson’s disease; bradykinesia, rest tremor, muscle rigidity, and postural instability. The degree of neuronal loss in this area also determines the severity of symptoms.
Other changes in the brain are also strongly related to signs and symptoms, including changes in the hippocampus and cholinergic cortical structures. Degeneration in these brain regions strongly contributes to the appearance of dementia in patients with Parkinson’s disease. Additional regions of the brain may also contribute to a lesser degree, including changes in the serotonin and noradrenaline pathways.
Two subtypes of Parkinson’s disease
Changes in the brain can also help to discriminate between two sub-types of Parkinson’s disease. The two sub-types are 1) tremor-dominant Parkinson’s disease and 2) postural instability and gait (or walking) difficulty Parkinson’s disease.
- Tremor-dominant. Changes in tremor-dominant Parkinson’s disease are found in the retrorubral A8 field in the midbrain.
- Postural instability. In those with posture instability and gait difficulty, lesions tend to occur in the substantia nigra and the locus coeruleus.
Timing of histopathological changes
Histopathological changes in the brain have also been linked to the order of symptom appearance in those with Parkinson’s disease. First, lesions appear on the dorsal nucleus of the vagus nerve and the olfactory bulb. Later, degeneration affects the substantia nigra and the locus coeruleus. Finally, there is a lesion of the cortical areas (particularly the entorhinal and cingulate cortices).
Another pattern of degeneration is described as cephalic progression. In the first stage, this starts in the peripheral and autonomic nervous systems. Later, in the second and third stages, lesions reach the brain stem. Lesions finally reach the superior cortical areas in the fourth and fifth stages.
The timing of histopathological changes can help conceptualize and perhaps explain the order of appearance of signs of Parkinson’s disease in the context of the terminology recommended by the Motor Disorders Society.
Stages of Parkinson’s Disease
The Movement Disorders society has recommended the following terminology for classifying the stages of Parkinson’s disease:
- Preclinical Parkinson’s disease. This phase can be described by the presence of the degeneration of the nervous system without the signs and symptoms of Parkinson’s disease. In this stage, the patient can only be assessed for possible risk factors because no clinical signs have appeared.
- Prodromal Parkinson’s disease. This phase can be described by the presence of early signs and symptoms of Parkinson’s disease. Signs and symptoms in this phase tend to be mild and subtle. Signs and symptoms are classically divided into motor (movement-related) and non-motor (non-movement related). It is important to note that this phase has also been termed the “pre-motor” phase.
- Clinical Parkinson’s disease. The diagnosis of Parkinson’s disease is possible in this phase due to the presence of the classical motor signs.
Risk Factors of Parkinson’s Disease
In order to achieve an early diagnosis of Parkinson’s disease, it is important to study the possible risk factors. These include:
- Age. Parkinson’s disease tends to manifest in the 5th and 7th decades of life. Tremor-dominant Parkinson’s disease develops earlier, typically in the 2nd and 4th decade of life. Posture instability and gait difficulty Parkinson’s disease tend to develop later, after the 6th decade of life.
- Sex. Another risk factor is being male. There are 3:2 males to females ratio for those that develop Parkinson’s disease.
- Hereditary. Hereditary risk factors include having a history of Parkinson’s disease in the family and specific genetic alterations. If a patient has a family history of the disease, their risk increases to three times higher than average. Also, genetic alterations put patients at higher risk than others. Some of the specific gene alterations include SNCA, LRRK2, GBA, PARK2, PINK1, and DJ1.
- Environmental. Environmental factors, such as head trauma and toxic exposure (in particular organophosphates and 1-methyl-1-phenyl-1,2,3,6-tetrahidropiridine) have been shown to increase the risk. In contrast, smoking, caffeine, alcohol, and elevated urate may actually decrease the risk.
Diagnosis of Parkinson’s Disease in the Prodromal Phase
During the preclinical phase, only risk factors can be studied in patients. Therefore, the diagnosis is only possible beginning in the prodromal phase. It is essential for the clinician to be meticulous while studying the patient to observe the subtle, early signs and symptoms of Parkinson’s disease. Note that even though the signs and symptoms of Parkinson’s disease are not as severe in this phase, the quality of life is affected.
There is still much research being conducted to discover which signs are the most useful in the diagnosis of Parkinson’s disease during the prodromal phase. The following have been shown to be useful in the early diagnosis:
- Olfactory dysfunction.
- Sleep disturbances
- Constipation
- Mild motor disorders
Olfactory dysfunction
- Olfactory dysfunction means difficulties with a sense of smell. It is one of the earliest signs and symptoms of Parkinson’s disease.
- There is no definite pathophysiological cause of this, currently. However, degeneration of the nerves in the olfactory bulb, olfactory nucleus, the amygdala, and the olfactory cortex could explain this dysfunction.
- Depending on its severity, it is called hyposmia or anosmia. Hyposmia refers to a partial loss of smell while anosmia refers to a complete loss of smell.
- Olfactory dysfunction can be identified through the patient’s medical history or certain medical tests.
- Olfactory dysfunction is a nonspecific sign, meaning the presence of this does not necessarily indicate that a patient has Parkinson’s disease. That being said, olfactory dysfunction is very prevalent in Parkinson’s disease patients. Its prevalence, ranging from 60 to 90%, is even higher than the major motor signs of Parkinson’s disease.
Sleep Disturbances
- Rapid eye movement sleep behavior disorder is a common sleep disturbance in those with Parkinson’s disease.
- Like anosmia and hyposmia, the mechanism responsible for this symptom has not been identified yet. However, it could be explained by lesions in the locus coeruleus, raphe nuclei, thalamus, and hypothalamus.
- Rapid eye movement sleep behavior disorder is characterized by violent dreams, vocalizations, loss of regular sleep, atony, and dangerous behaviors during sleep.
- This sign is quite useful in diagnosing Parkinson’s disease because it is highly specific to neurodegenerative processes. Studies have shown that patients with rapid eye movement sleep behavior disorder have a 50-70% risk of neurodegenerative disease and at least 38% will be diagnosed with Parkinson’s disease. However, it does not distinguish which neurodegenerative disease is present.
- Clinically, it can be identified through patient history or an assessment questionnaire.
Constipation
- Constipation is a key sign in the early detection of Parkinson’s disease. This sign can be identified from 2 months up to 24 years before the appearance of the motor signs required for Parkinson’s disease diagnosis.
- Constipation can be the result of the initial neurodegeneration in the autonomic nervous system. In about 60-70% of patients, the autonomic nervous system has alfa-synuclein inclusions.
Minor motor disorders
- There are motor signs that can aid in the early diagnosis of Parkinson’s disease.
- Micrographia has been a minor sign in the clinical phase for a long time, but recently it has been used as a tool to identify patients in the Prodromal phase.
- Micrographia is defined as progressively small handwriting that continues to diminish in size until it is unreadable.
- It has been suggested that patients be studied for dysgraphia rather than micrographia because this would allow a richer exploration of the patient’s condition.
- When examining a patient for dysgraphia, more components of handwriting are analyzed, including size, duration, speed, and fluency.
- It is important to note that micrographia or dysgraphia are associated with one of the cardinal signs of Parkinson’s disease, bradykinesia. Bradykinesia, strictly speaking, does not appear until the clinical phase begins along with the other cardinal signs.
Other Parkinsons Disease Symptoms
Signs of Parkinson’s Disease
The cardinal motor signs of Parkinson’s disease are determined by the level of degeneration in the substantia nigra. They are:
1. Bradykinesia
- Bradykinesia is a frequent manifestation among the diverse signs and symptoms of Parkinson’s disease.
- Bradykinesia, hypokinesia, and akinesia are symptoms characterized by slowness or failure to perform motor functions in general. However, it is important to note that each has a precise clinical definition.
- Bradykinesia is defined as the slowness of movement, akinesia is defined as the absence of movements, and hypokinesia is described as smaller movements than normal movements.
- These motor symptoms can manifest also in day to day activities. These include partial or complete loss of facial expression (hypomimia or amimia), reduced volume of speech (hypophonia), alteration of writing (micrographia or agraphia), and drooling (sialorrhea).
- These manifestations are some of the best-understood signs and symptoms of Parkinson’s disease, as they are related to the simple, direct and indirect motor control pathways.
2. Resting Tremor
- Even though there are several types of tremors, resting tremor stands out because it frequently occurs in Parkinson’s disease.
- Resting tremor is defined as an asymmetric tremor of moderate amplitude in agonist-antagonist alternating contractions.
- Common movements in resting tremor include hand movements (sometimes called the pill-rolling tremor), leg abduction-adduction tremor, and head movement (movements resembling yes or no gestures).
3. Rigidity
- Rigidity is defined as an increase in muscle tone.
- It is identified upon palpation of the muscle at rest and resistance to passive movements.
- A remarkable clinical finding is cogwheel phenomena. This sign is the consequences of two overlapping cardinal signs, rigidity, and tremor. The cogwheel phenomena can be described as resistance in passive movement.
4. Postural Instability
- Physiological posture neurological systems are deficient due to decreased or loss of postural reflexes.
- It is of great clinical relevance because it is associated with falls in elderly patients.
- Other signs associated with this cardinal sign are gait disturbances, including the freezing of gait and shuffling gait, both of which have been associated with previously mentioned signs (akinesia and hypokinesia).
- Freezing of gait is defined by the difficulty of gait initiation and unintentional motor blocks during walking. Shuffling gait is characterized by short and quickly alternating steps.
Non-Motor Signs of Parkinson’s Disease
Non-motor signs can be displayed in the clinical phase of Parkinson’s disease. These include:
- Psychiatric manifestations
- Autonomic dysfunction
- Sleep disorders
- Olfactory dysfunction
- Pain and cognitive impairment
Among these non-motor signs, psychiatric manifestations and cognitive impairment need special consideration. These symptoms are diverse. They often require referral to specialists to distinguish non-motor manifestations of Parkinson’s disease from coexisting neuropsychiatric diseases. Also, it is important to know that these signs are evidence of progression to the final stages of Parkinson’s disease. They are easily identified as they are incapacitating and severely detrimental to the quality of life of the patient.
Parkinson’s disease is progressive and irreversible in nature. Therefore, a precise and early diagnosis of this illness is critical. Essential to this is knowing the underlying pathophysiological mechanisms that occur during the course of the disease. It is evident that our current understanding is lacking. This could explain the lack of testing technologies for early diagnosis, which could aid in the clinical study of patients at risk. Also, it explains the difficulty of understanding the heterogeneity in the signs and symptoms of Parkinson’s disease. However, until more research is done, it is the signs and symptoms of Parkinson’s disease and the detailed study of patients in the three phases (preclinical, prodromal, and clinical phases) which will provide the best outcomes for patients.