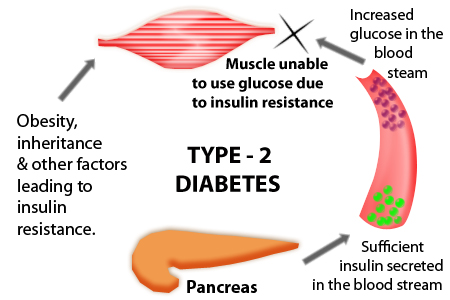
Type 2 diabetes is a chronic disease with a high risk of complications in patients. Nevertheless, this can be prevented with early diagnosis and adequate management. Management of type 2 diabetes must be integral and comprehensive in order to be successful. This could be considered the other side of the multifactorial causes of type 2 diabetes. In order to stop or perhaps in the future reverse the process ongoing in type 2 diabetes, one must address many factors.
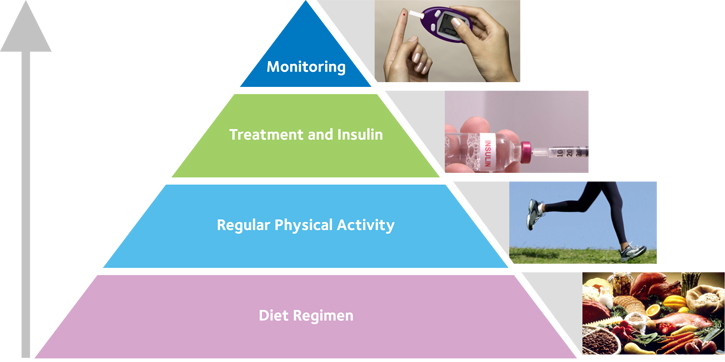
Table of Contents
Type 2 Diabetes Treatment
In order to organize the treatment of type 2 diabetes, specific goals must be established. Based on these goals physician must design a treatment plan that must include non-pharmacological and pharmacological intervention. Currently, even surgical options are considered when treating type 2 diabetes.
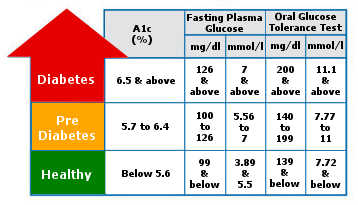
It has been observed that patients with unstable glycemic levels tend to develop more complications than patients who do. For these reasons, a physician needs to establish goals when treating type 2 diabetes. It is essential in order to evaluate if the therapy is being successful. While there are many things to consider when establishing a goal, it will always revolve into making sure the sugar levels are stable in the patient. Additionally, the values chosen as the goal will depend on the type of test used in each person. The test normally used to determine if the patient is within the recommendation are the glycosylated hemoglobin test, preprandial capillary plasma glucose, and peak postprandial capillary plasma glucose.
In general, the recommended values according to the Standards of Care for each of the different measurement are the following
- glycosylated hemoglobin test – less than 7 %
- preprandial capillary plasma glucose – values ranging from 80 to 130 milligrams per deciliter
- peak postprandial capillary plasma glucose – less than 180 milligrams per deciliter
However, each physician must be aware that these are only guidelines and glycemic goals may vary according to the physician´s criteria and each individual case. Factors such as the risk of hypoglycemia, duration of the disease, life expectancy and many other will determine if goals should be more or less stringent. This is because some of these factors are associated with the worst outcome with stringent goals and the associated intense treatment of type 2 diabetes.
Glycemic goals can be more stringent according to factors that are usually modifiable or factors that are potentially modifiable. Among factors that allow for stringent goals are a risk of hypoglycemia, recently diagnosed diabetes, long life expectancy, absences of important comorbidities, and absence of vascular complications. Factors that are potentially modifiable that allow for stringent goals are high motivation, patient´s adherence, self-care capacity and accessibility to resources and support system. On the other hand, the opposite of these factors requires the establishment of less stringent goals.
Nonpharmacological Treatment of Type 2 Diabetes
Upon the establishment of the individual glycemic goal for the patient, the physician can move on to the formulation of the treatment plan. The basis of this plan should be the nonpharmacological treatment of type 2 diabetes. It is important to point out that the nonpharmacological aspect of type 2 diabetes management in most cases will not vary due to glycemic goals. These are recommendations and part of the management that should always be present in the treatment of patients.
1. Nutrition & Diet
The most basic aspect of the nonpharmacological treatment is the Medical Nutrition Therapy program and the nutritional advice given by the physician. The Medical Nutrition therapy program should be prepared by a registered dietitian. The dietitian when planning this program should take into consideration the type of therapy administered. This is particularly relevant when planning meals for a patient using insulin therapy. Additionally, the risk of hypoglycemia is another aspect that needs to be considered when planning a program like this. Finally, the recommendations given to the patient by both the physician and the dietitian need to be congruent to ensure adherence and the patient´s trust in the health care professionals.
The plan and recommendation should deal with the following aspect of the patient’s diet: the energy balance, eating patterns, macronutrient distribution, macronutrient specific details, and reduction of both sodium and alcohol. The energy balance of a patient will be oriented around satisfying the patient’s nutritional needs and if the patient needs to lose weight. Progressive weight loss can be achieved through adjustments in the energy balance of a patient. With respects to the macronutrient distribution and their details, there are no specific percentages of fat, proteins, and carbohydrates rather special considerations need to be taken for each type of macronutrient. For example, patients should be oriented to consume carbohydrates coming from foods with a low glycemic index and high content of fiber. Carbohydrates sources containing sugars should be avoided. The ideal fat content is currently inconclusive but healthy choices of fat are evident. Particularly, food which contains long-chain omega-3 fatty acids such as fatty fish, nuts, and seeds.
Alcohol and Sodium restriction
The other nutritional recommendations include the restriction of both alcohol and sodium. The need for moderate alcohol consumption is evident but aside from its moderation, patients need to be aware alcohol can induce delayed hypoglycemia. Additionally, sodium should be restricted to less than 2,300 milligrams per day. However, this value can be lowered in case patients diagnosed with both diabetes and hypertension.
2. Physical Activities.
In addition to nutrition, the recommendation of physical activities is also an essential part of the nonpharmacological treatment of type 2 diabetes. The Standards of Care indicate children should engage in at least 60 minutes of physical activities daily. Adults engage in at least 150 minutes per week of aerobic physical activity. (There should not be more than 2 consecutive days without exercise). Additionally, if patients do not have contraindications, adults should perform at least 2 resistance routines per week. Also, throughout the day if patients spend more than 90 minutes in sedentary activity, they should try to divide and reduce this time.
Pharmacological Treatment of Type 2 Diabetes
To aid the nonpharmacological treatment of type 2 diabetes, the physician could prescribe several types of pharmacological options. The Standards of Care suggest that at first pharmacological treatment of type 2 diabetes should be composed of a single pharmacological agent, metformin.
However, if the patient does not reach the proposed glycemic goal after 3 months of monotherapy, the physician can add other pharmacological options. Initially, only one pharmacological agent is added but a third agent can be chosen if the patient doesn’t the target isn’t reached after 3 months of dual therapy. Finally, if a patient does not reach the goal in 3 months of triple therapy, then a final combination of injectable therapy is suggested.
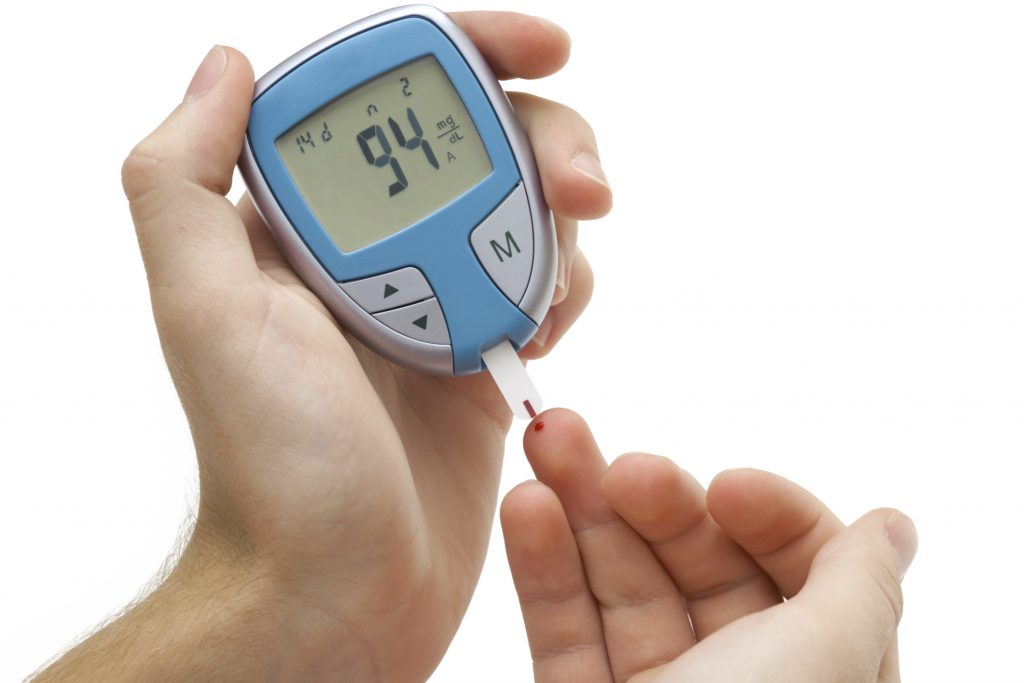
Regular Glucose level blood test is a must
Among the currently available pharmacological agents, which are used for type 2 diabetes treatment, are metformin, sulfonylureas, thiazolidinediones, glucagon-like-peptide-1 receptor agonist, dipeptidyl peptidase 4 inhibitors, sodium-glucose transporter-2, and insulin. Each of these glucose-lowering agents has its own mechanism of action and special characteristics of vital importance when determining which agent to use. These characteristics include efficacy, hypoglycemia risk, the effect of on the patient’s weight, side effects, and economic cost.
1. Metformin
Metformin is the basic pharmacological treatment of type 2 diabetes and it is recommended that it should be used in all combinations. It comes from a group of glucose-lowering agents called biguanides which lower hepatic glucose production, possibly through the activation of AMP-kinase enzyme. It an agent with extensive use, which usually does not present with hypoglycemia. Additionally, it promotes weight loss in patients and has a low economic cost.
2. Sulfonylureas
Other groups of therapeutical agents are sulfonylureas, which function by increasing insulin secretion as a result of closing potassium-ATP channels on the pancreatic beta cells. It is another agent with extensive use and low economic cost but it can produce hypoglycemias. Additionally, there is another group of agents called the meglitinides which have the same mechanism of actions and related characteristics.
3. Glucagon-like-peptide-1 receptor agonist & Dipeptidyl peptidase 4 inhibitors
Type 2 diabetes treatment also include agents that affect the incretin signaling pathway. These agents include two groups, the glucagon-like-peptide-1 receptor agonists, and the dipeptidyl peptidase 4 inhibitors. While both increase insulin secretion, one does this by activating a receptor in the pancreatic beta-cell while the other inhibits an enzyme which degrades the molecular signal which activates the receptor. Both are novel treatment options that do not produce hypoglycemia but carry the high economic cost for patients.
4. Thiazolidinedione
Another pharmacological group used in the treatment of type 2 diabetes is the thiazolidinedione. These pharmacological agents increase insulin sensitivity by activating the peroxisome proliferator-activated receptor-gamma transcription factor. It relatively new treatment option without hypoglycemic risk and low economic cost.
5. Sodium-glucose transporter 2 inhibitors
A novel group in the pharmacological management of type 2 diabetes the sodium-glucose transporter 2 inhibitors. This group inhibits a glucose transporter in the kidney responsible for the reabsorption of glucose. Resulting in renal losses of glucose which lower the serum concentration of glucose. They have several additional effects including lowering a patient’s pressure and weight. Also, they do not cause hypoglycemia. However, they can cause hypotension and are quite expensive.
6. Insulin
Finally, insulins are pharmacological options in type 2 diabetes treatment. The effects of insulin are numerous and they bind the insulin receptors found in the body. All insulins have a risk of inducing hypoglycemia but their cost can vary because there are different types of insulin. Usually, the insulins are grouped according to how fast they can act as rapid-acting, short-acting, intermediate and long-acting. This classification is relevant to the different insulin treatment scheme currently.
Additional to the progression from monotherapy to combined therapy, the way insulin is administered can be adjusted to improve results. This scheme will be affected by the complexity, the amounts of injections, and the flexibility of each.
The simplest scheme is the basal insulin, in which intermediate insulins are administrated once, usually along with metformin and some other glucose-lowering agent. If the patient does not reach the goal another schema can be used. The other schema begins to add to the complexity and a number of injections. One option is the addition of a rapid insulin injection before the largest meal along with the previous basal insulin. The other option is the administration of premixed insulin twice a day. Finally, there is the “basal-bolus” schema in which 2 or more rapid insulin injections are administered before meals along with basal insulin administration.
Bariatric surgery
Another treatment option for patients diagnosed with type 2 diabetes is using bariatric surgery. It should be considered for patients with a body mass index above 35 kilograms per meter squared. Special consideration is taken for patients who have associated comorbidities and other management options are not being efficient. It has been observed that patients with bariatric surgery have seen benefits in their glycemic control. Nevertheless, further research is needed to recommend bariatric surgery who do not meet the regular obesity criteria. Additionally, this is a surgery with risk and the physician should keep this in mind before recommending it.
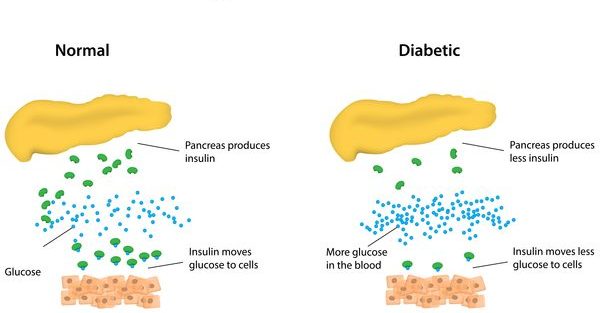
Physicians and patient´s alike must be aware that all of these treatments for type 2 diabetes are not a cure for the disease itself. It is important to recall that in type 2 diabetes there is a hyperglycemic state with insulin dysfunction which can be stabilized but the underlying changes will remain. Therefore, treatment options are not the cure for type 2 diabetes rather measure which will control the disease and the complications arising from this disease.
However, novel treatment options are being developed that could become a cure for type 2 diabetes. In some research, strict dietary controls led to an increase in the incidence of diabetes within the population studied. Yet these options need further research before considering them as the definitive cure.
Until these are further developed and studied, current nonpharmacological and pharmacological treatments will remain for the treatment of type 2 diabetes. Which might not reverse the process causing the illness in the patient but will be able to control the complications. This should not be taken lightly or belittled because the quality of life of patients and the economic cost these complications carry are very significant.
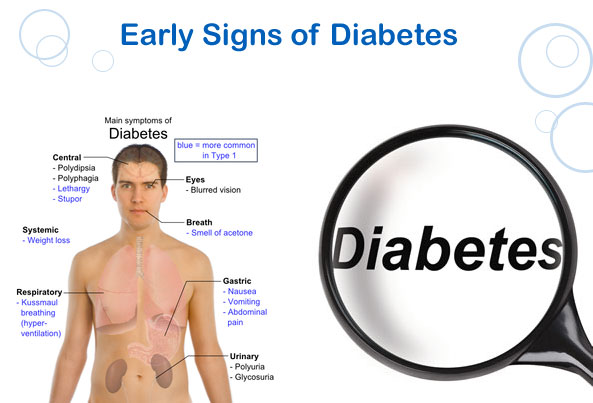
Of equal importance are the screening efforts and early diagnosis of the disease which will allow patients earlier access to treatment options. Early access will increase the patient’s outcome and possible for a healthier and rewarding life.
When a person is diagnosed with type 2 disease, support from friends and family is also very important. The people that suffer from this chronic disease can often become depressed and are suffering from anxiety. This is why it is highly important that these people have the support of their beloved ones.