Paresthesia is a temporary or long-term alteration in local sensibility and the patient can describe it as numbness, tingling or as a pins and needles sensation. (1) Paresthesia can come as a side effect among people with fibromyalgia. However, there is no veridic study to link the personality traits in fibromyalgia with paresthesia. (2)



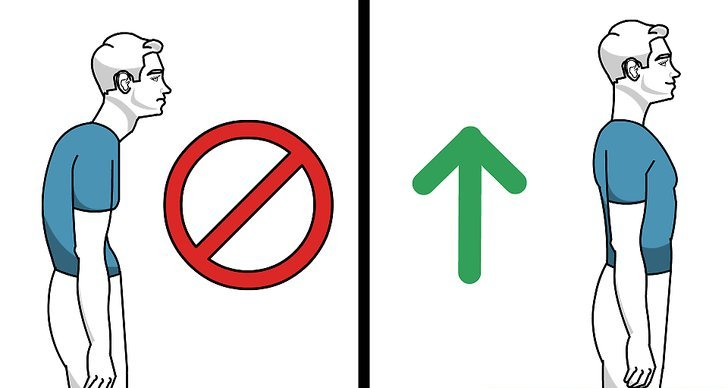
Most people go through the usual “pins and needles” feeling. This is temporary paresthesia and can come as a result of sitting too much with your legs crossed or falling asleep with one arm crooked under your head. Mainly, it happens when a nerve has to take too much exterior pressure from an unfortunate posture. Temporary paresthesia of this kind quickly washes away when the nerve is free from the pressure. (3)
Table of Contents
Chronic paresthesia and its multiple causes
Chronic paresthesia might imply some serious problems that you need to see a doctor about because it might hide serious neurological afflictions and even grave nerve damage. Some of the most frequent causes of chronic paresthesia are as follows:
- Disorders of the central nervous system: strokes, sclerosis, traverse myelitis, enchephalitis
- A tumor
- A vascular lesion pressed against the brain
- A vascular lesion pressed against the spinal cord
- Carpal tunnel syndrome or other nerve entrapment syndromes (3)
Temporary paresthesia and its underlying causes
The peripheral sensory nerves take our sensations to our spinal cord. From here, these signals get on a journey to the brain helped by the trigeminal nerve and brain stem. Anything that goes wrong on this “road” can lead to paresthesia. The first symptoms of transient paresthesia are well-known to you, as well as to any human being: that sudden burning sensation followed by numbness, tingling and a thousand pins and needles in your affected body part, which is usually an extremity. These temporary feelings can occur from a simple thing like sitting with your legs crossed or sleeping on your arm or in a wrong position. So, the causes of this temporary cause of paresthesia can be put into categories such as:
- Obdormition: numbness caused by a prolonged pressure on a nerve, as in sitting with your legs crossed for a long time
- Whiplash injury can cause an upper extremity paresthesis. Whiplash is a type of of injury that took place in the cervical soft tissue. There is an incidence of 13% whiplash patients manifesting paresthesia as well. Full recovery only happens after 6 months or so of injury
- Hyperventilation syndrome can cause paresthesia in 35% of the cases. Paresthesia can easily occur after as little as three minutes of hyperventilation.
- Panic attack can cause temporary paresthesia of the mouth, hands and feet. Actually, paresthesia is a common indicator of severe panic attacks and should be taken seriously
- TIA, aka Transient Ischemic attack caused by afflictions such as thrombosis, embolus, intravascular debris and blood vessels disruption can also lead to paresthesia.
- Seizures: This is one common cause of paresthesia which can occur during a seizure or after, as a side-effect. Even the vagus nerve stimulation treatment of seizures can lead to temporary paresthesia.
- Dehydration is also a cause of temporary paresthesia. It might come as the most unexpected one for you and we understand it, but dehydration is a serious issue and should not be messed with. When there is an accumulated 5-6& of water loss, paresthesia is triggered. So, keep hydrated! (5)
Diagnostic evaluation in case of paresthesia
Normally, what paresthesia does is block the sensory pathways between the peripheral sensory nervous system and the sensory cortex. In neurology practice, the most important diagnostic tool used is a thorough medical history, “which properly reflects the true nature of what the patient is experiencing, provocateurs, precipitating and relieving factors, concomitant illnesses, such as diabetes.” (4)
That is to say, the patient will go through a preliminary medical history, a thorough physical examination and laboratory tests to come to the final diagnosis. Additional tests might be recommended by the doctors, depending on the result of the above examinations, like:
- Nerve conduction study to measure how fast nerve impulses travel inside the muscles
- Electromyography, testing the electrical activity of the nerves and muscles interacting with each other
- Magnetic resonance imaging to look more in detail at different body areas
- Ultrasound to produce images of body areas and phenomena such as the nerve compression
All in all, paresthesia can be a serious issue if not treated seriously.