Tendinopathy is a common condition affecting 2-5% of the general population. The risk of tendinopathy is higher in athletes with roughly 50% of all sports injuries being tendon injuries.
What is Tendinopathy?
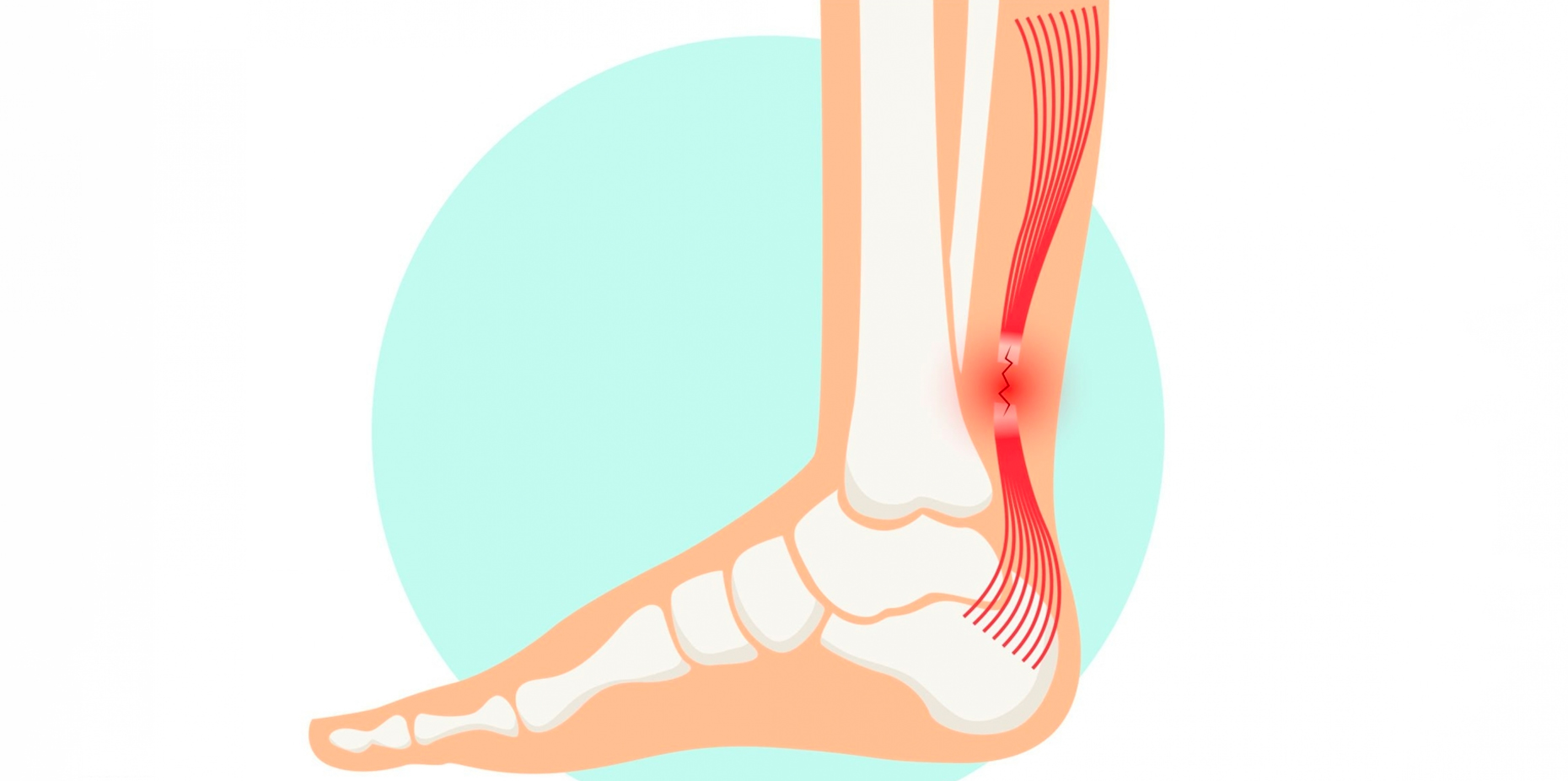
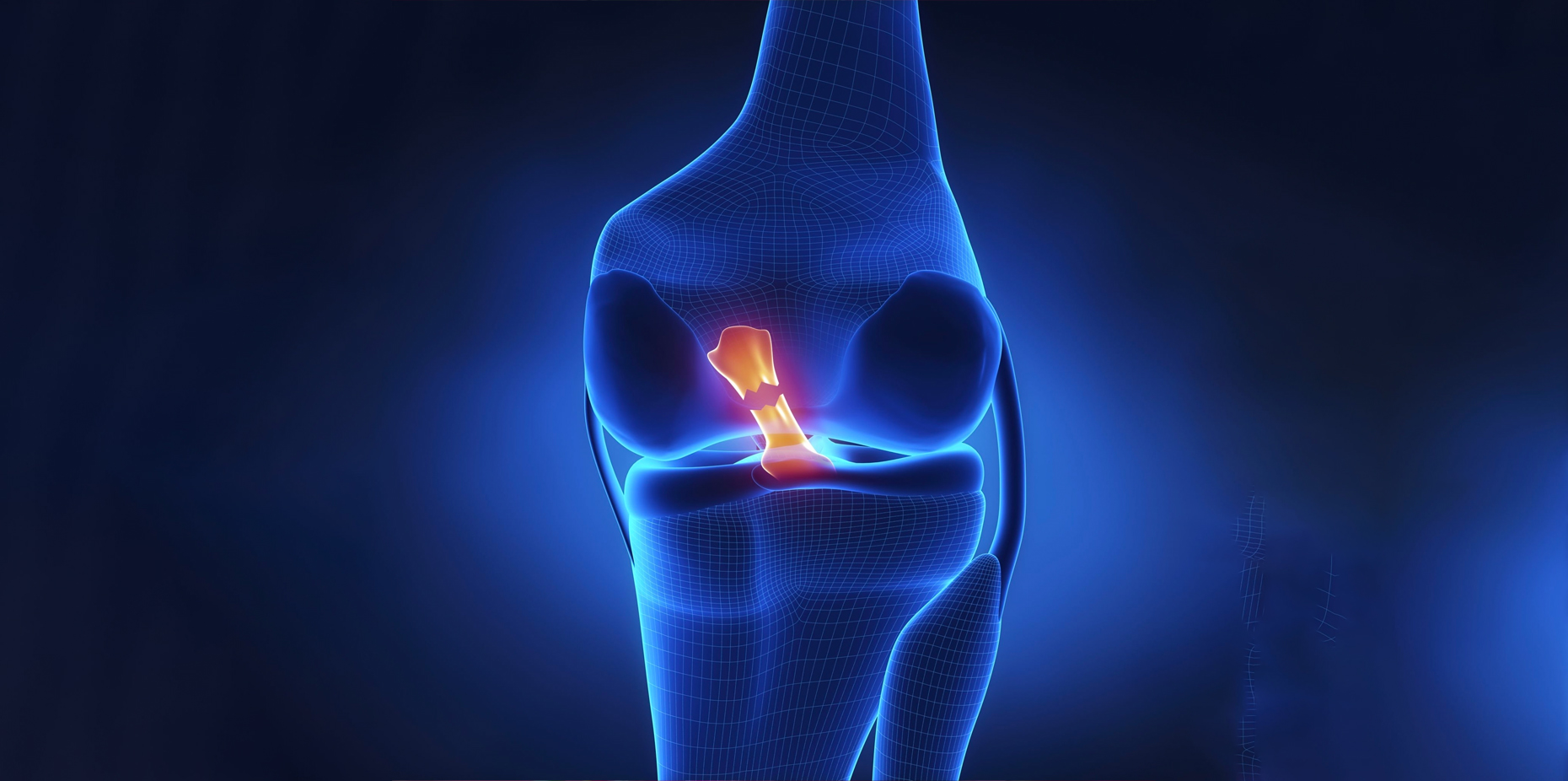
Tendinopathy is a broad term that encompasses a group of tendon-related disorders. Tendons are tough, flexible bands of tissue that connect muscles to bones, enabling joint movement. When tendons become injured or damaged, tendinopathy can occur. It’s important to note that tendinopathy is not synonymous with tendonitis, as the latter specifically refers to inflammation of a tendon. Tendinopathy, on the other hand, involves a degenerative process that includes changes in the tendon’s structure and composition.
Symptoms
The symptoms of tendinopathy can vary depending on the specific tendon affected and the severity of the condition. However, there are common symptoms that individuals with tendinopathy often experience. These symptoms include:
- Pain is the hallmark symptom of tendinopathy which usually starts as a dull, achy sensation around the affected tendon and is aggravated by movement or activity. Pain may also increase after periods of rest or inactivity.
- Tenderness around the affected tendon with palpation
- Stiffness in the affected joint making movements feel restricted or uncomfortable, especially in the morning or after inactivity
- Mild to moderate swelling around the affected tendon as a result of the body’s inflammatory response to the tendon’s degenerative changes
- Reduced range of motion and decreased flexibility with limited range of motion in the joint associated with the affected tendon
- Weakness due to the tendon’s structural integrity being compromised which can impact the affected limb’s overall functionality and performance
- Crepitus (a crackling or grating sensation) that can sometimes be felt or heard when moving the affected joint, caused by friction between the degenerated tendon and surrounding tissues
It’s important to note that tendinopathy symptoms can develop gradually over time, and they may not be severe initially. Ignoring early symptoms or pushing through pain during activities can potentially worsen the condition. If you suspect you might have tendinopathy, it’s advisable to seek medical attention for a proper diagnosis and appropriate management to prevent further complications and promote healing.
Causes
Tendinopathy can result from a combination of intrinsic and extrinsic factors that contribute to the degeneration and damage of tendons. Understanding these causes is essential for preventing, diagnosing, and effectively managing the condition. Here are some of the key causes of tendinopathy:
- Overuse: activities that involve frequent and repetitive motions can strain the tendon, leading to microtrauma and degeneration over time. Athletes, especially those who engage in sports that require repetitive movements (such as runners, tennis players, and golfers), are at higher risk (1).
- Age: as individuals get older, tendons become less elastic and more prone to damage. This degeneration is a normal part of the aging process, but it can be exacerbated by other factors like poor nutrition, lack of exercise, smoking, and certain medical conditions (2).
- Poor mechanics: incorrect biomechanics and poor posture during physical activities can put undue stress on tendons, increasing the risk of tendinopathy. For example, improper running form or lifting technique can strain the tendons, leading to injury.
- Vascular issues: tendons require a good blood supply for proper healing. Reduced blood flow to a tendon can hinder its ability to repair and regenerate, making it more susceptible to damage and tendinopathy.
- Genetics: some individuals might have a genetic predisposition to developing tendinopathy due to variations in the genes responsible for collagen synthesis and tendon structure. Genetic factors can influence the strength and resilience of tendons.
- Training errors: abruptly increasing the intensity, duration, or frequency of physical activity without proper conditioning can place excessive strain on tendons, leading to microtrauma and potential tendinopathy.
- Occupational factors: certain occupations that involve repetitive movements, heavy lifting, or awkward postures can contribute to the development of tendinopathy. Jobs that require repetitive motions, such as typing or manual labor, can stress the tendons over time (3).
- Previous injuries: tendons that have previously been injured or experienced trauma are more vulnerable to developing tendinopathy. Improper healing or scar tissue formation from previous injuries can compromise the tendon’s integrity.
- Medical conditions: certain medical conditions, such as diabetes, rheumatoid arthritis, and metabolic disorders, can weaken tendons and increase the risk of tendinopathy. These conditions can impair the body’s natural healing processes and compromise tendon health.
- Medications: long-term use of certain medications, such as fluoroquinolone antibiotics and corticosteroids, has been associated with an increased risk of tendinopathy due to their potential impact on tendon health and structure (4).
It’s important to recognize that tendinopathy is a multifactorial condition, often resulting from a combination of these factors. Reducing the risk of tendinopathy involves maintaining a healthy lifestyle, practicing proper biomechanics during physical activities, and addressing any underlying medical conditions that could contribute to tendon damage.
Summary: The caues of tendinopathy is multifactorial and involves a combination of overuse, age, genetics, training erros, medical conditions, and medication side effects.
Diagnosis
Accurate diagnosis is crucial for effective management of tendinopathy. Healthcare professionals often employ a combination of the following methods to assess the condition:
- Clinical history: understanding the patient’s medical history, activity level, and potential contributing factors is essential for a comprehensive diagnosis.
- Physical examination: a comprehensive assessment of the affected area, including palpation, range of motion tests, and strength assessments, can provide valuable insights into the nature and extent of the tendinopathy.
- Functional tests: assessing how the patient performs specific movements or activities can aid in determining the impact of tendinopathy on their daily life.
- Imaging: X-rays can help rule out other conditions, while ultrasound and MRI scans offer detailed views of the tendon’s structure, helping to identify degenerative changes.
Treatment Options
Tendinopathy management typically involves a multifaceted approach that addresses pain relief, tendon healing, and prevention of recurrence. Treatment options range from conservative measures which are more common, to more invasive interventions which are utilized when conservative measures fail to address symptoms:
- Rest and activity modification: initially, resting the affected tendon and modifying activities to reduce strain is crucial. This allows the tendon time to heal and prevents further damage.
- Physical therapy: targeted exercises can help improve tendon strength, flexibility, and biomechanics. Eccentric exercises, which involve lengthening the tendon during contraction, are commonly used to stimulate tendon healing.
- Pain management: nonsteroidal anti-inflammatory drugs (NSAIDs), ice packs, and topical treatments can provide short-term relief from pain and inflammation.
- Bracing and taping: supportive braces or taping techniques can help alleviate stress on the affected tendon during activity.
- Corticosteroid injections: in some cases, corticosteroid injections may be considered to alleviate pain and inflammation. However, these should be used judiciously due to potential long-term side effects.
- Platelet-Rich Plasma (PRP) therapy: this emerging treatment involves injecting a concentrated solution of the patient’s own platelets into the affected tendon, potentially promoting healing (5).
- Surgery: surgical intervention is typically considered when conservative treatments fail or if there is a significant tendon tear. Surgical procedures can involve tendon repair, removal of damaged tissue, or in severe cases, tendon grafting.
Summary: Tendinopathy is most often treated conservatively with activity modification, pain management, physical therapy, and bracing. If conservative measures fail, options include corticosteroid injection, PRP, or surgery.
Conclusion
Tendinopathy is a common condition involving chronic tendon pain and degeneration. Symptoms include pain, tenderness, stiffness, reduced range of motion, weakness, and decreased function. Diagnosis of tendinopathy is done through a combination of medical history, physical examination, functional tests, and imaging. Conservative treatment is usually successful and includes activity modification, physical therapy, pain management and bracing/taping. If conservative treatments do not address symptoms fully, procedures such as corticosteroid injections, PRP, or surgery may be used.