Diabetes affects approximately 422 million individuals globally, with most residing in low- and middle-income nations. Sadly, around 1.5 million deaths are directly linked to this condition each year (1).
Table of Contents
What is Diabetes?
Diabetes is a group of conditions that affect the body’s ability to utilize blood sugar (glucose) effectively. Glucose serves as a vital energy source for the cells in muscles and tissues. It is also the primary fuel for the brain (2).
The causes of diabetes may vary depending on the type. However, regardless of the type, diabetes results in elevated levels of sugar in the blood, which might lead to serious health complications. There are several chronic forms of diabetes, including type 1 and type 2 diabetes. Additionally, there are potentially reversible conditions such as prediabetes and gestational diabetes (3).
Types of Diabetes
Diabetes is a condition that affects millions of people worldwide. It occurs when the level of glucose (sugar) in the blood is too high. There are several types of diabetes, each with its own causes and characteristics.
Type 1 Diabetes
Type 1 diabetes is a condition where the body is unable to produce insulin, a hormone essential for regulating blood sugar levels. This occurs because the immune system mistakenly attacks the cells in the pancreas responsible for insulin production (4). Without insulin, glucose cannot enter the body’s cells to provide energy, resulting in elevated blood sugar levels. This type of diabetes requires lifelong management through insulin therapy (5).
Type 2 Diabetes
Type 2 diabetes is the most common form of diabetes, accounting for around 90% of cases (6). In type 2 diabetes, the body either becomes resistant to the effects of insulin or doesn’t produce enough insulin to maintain normal blood sugar levels (7). Risk factors for type 2 diabetes include genetics, lifestyle factors such as diet and physical activity, and obesity (8). Without proper management, type 2 diabetes may lead to serious complications affecting the eyes, heart, and other organs.
Gestational Diabetes
Gestational diabetes develops during pregnancy in women who have not previously had diabetes (9). It is characterized by high blood sugar levels and requires careful monitoring and management to ensure the health of both the mother and the baby. Gestational diabetes typically resolves after childbirth but increases the risk of developing type 2 diabetes later in life (10).
Other Types of Diabetes
Apart from type 1, type 2, and gestational diabetes, there are less common forms of the condition. These include:
- Monogenic Diabetes: Caused by a single gene mutation, leading to conditions such as neonatal diabetes mellitus and maturity onset diabetes of the young.
- Cystic Fibrosis-Related Diabetes: Occurs as a complication of cystic fibrosis.
- Type 3c Diabetes: Also known as pancreatogenic diabetes, it might develop due to pancreatic damage resulting from surgery, injury, or illnesses like pancreatitis (11).
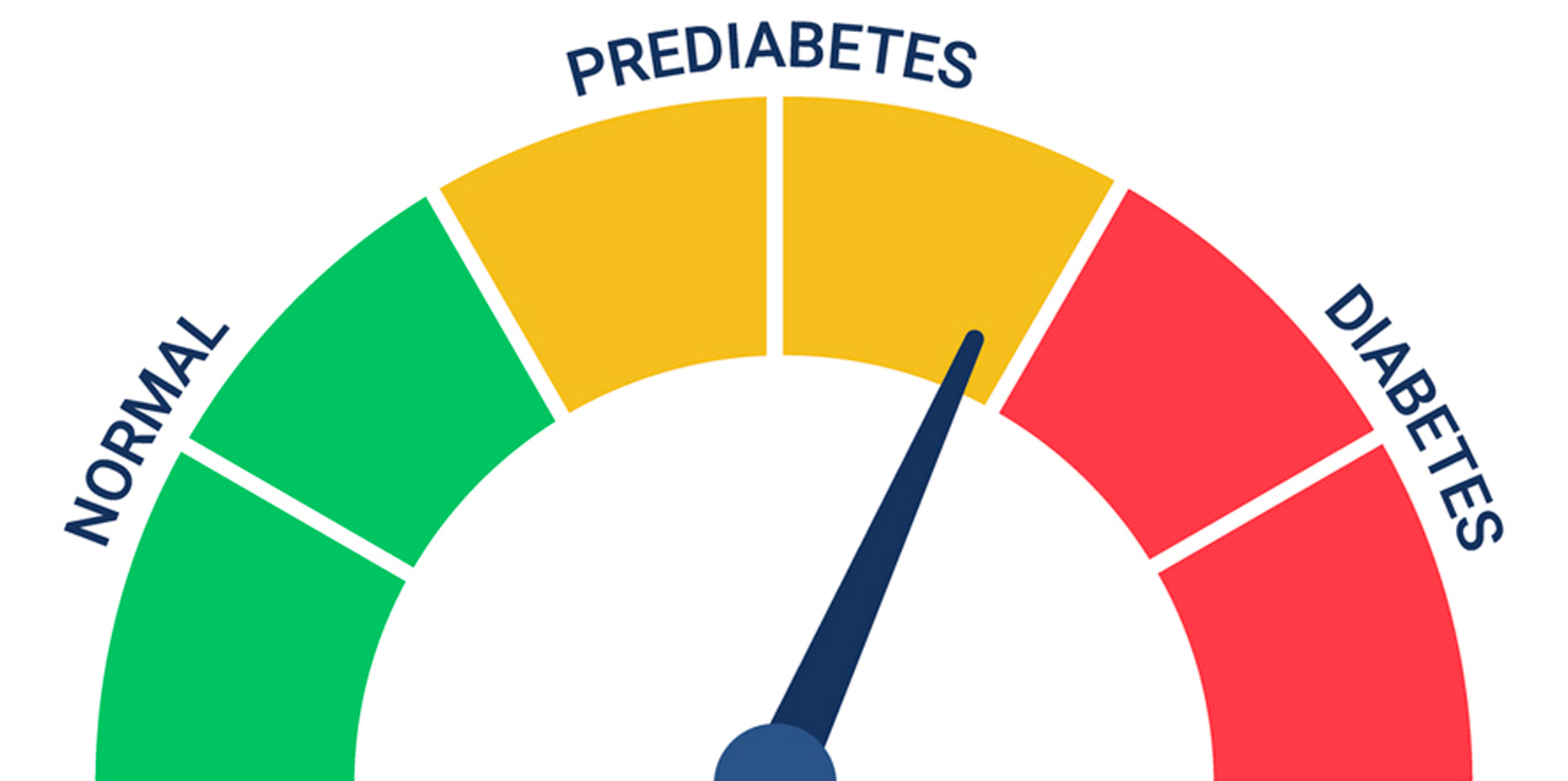
Prediabetes
Prediabetes is a condition in which blood sugar levels are higher than normal but not yet high enough for a diagnosis of type 2 diabetes. It significantly increases the risk of developing type 2 diabetes, as well as heart disease and stroke. However, lifestyle changes such as diet and exercise may help prevent or delay the onset of type 2 diabetes in individuals with prediabetes (12). It is crucial to raise awareness about prediabetes, as many affected individuals may not be aware of their condition.
It’s important for individuals to be aware of the different types of diabetes, their risk factors, and the importance of early detection and management in order to prevent complications and lead a healthy life. If you suspect you may have diabetes or prediabetes, it’s essential to consult a healthcare professional for proper evaluation and guidance.
Symptoms of Diabetes
The signs and symptoms of diabetes may vary depending on the level of blood sugar. Some individuals, particularly those with prediabetes, gestational diabetes, or type 2 diabetes, may not experience any noticeable symptoms. However, in type 1 diabetes, symptoms typically emerge rapidly and are often more pronounced.
Common signs and symptoms of both type 1 and type 2 diabetes include:
- Frequent Urination: Needing to urinate more frequently (13).
- Increased Thirst: Feeling thirstier than usual.
- Presence of Ketones in Urine: Ketones, produced when the body breaks down muscle and fat due to insufficient insulin, may be detected in the urine (14).
- Fatigue and Weakness: Feeling tired and weak (15).
- Mood Changes: Experiencing irritability or other mood fluctuations (16).
- Unintended Weight Loss: Losing weight without trying (17).
- Slower Healing Sores: Wounds taking longer to heal (18).
- Blurry Vision: Experiencing vision problems (19).
- Increased Susceptibility to Infections: Developing more infections, such as skin, gum, or vaginal infections (20).
Type 1 diabetes may onset at any age but is often diagnosed during childhood or adolescence (21). On the other hand, type 2 diabetes, which is more prevalent, might develop at any stage of life. While it’s more commonly diagnosed in individuals over 40, the incidence of type 2 diabetes in children is rising (22).
Causes and Risk Factors of Diabetes
Understanding the causes and risk factors of diabetes is crucial for managing and preventing this chronic condition. Let’s dive into the factors that contribute to the development of diabetes.
Causes
The underlying causes of most types of diabetes remain a subject of ongoing research. However, it is widely recognized that inadequate insulin production is a common denominator across various diabetes forms. Type 1 and type 2 diabetes, the two primary classifications, are believed to stem from a combination of genetic predisposition and environmental triggers. Despite extensive studies, the specific factors triggering diabetes onset remain unclear.
Risk Factors
The risk factors associated with diabetes vary depending on the type of diabetes under consideration.
- Family History: A familial predisposition to diabetes is observed across all types. Individuals with a family history of diabetes are more likely to develop the condition themselves. In some cases of type 1 diabetes, specific immune system cells known as autoantibodies are detected in family members, indicating an increased risk of developing the disease. However, it is essential to note that not all individuals with these autoantibodies will necessarily develop diabetes (23).
- Race and Ethnicity: Certain racial and ethnic groups exhibit a higher susceptibility to type 2 diabetes. Among these groups are Black, Hispanic, American Indian, and Asian American populations. While the reasons behind these disparities remain unclear, they underscore the importance of considering racial and ethnic backgrounds in diabetes prevention and management efforts (24).
- Environmental Influences: Environmental factors play a significant role, particularly in type 1 diabetes. Factors such as geography and exposure to certain environmental elements may contribute to the risk of developing the condition. However, the precise mechanisms through which these factors influence diabetes susceptibility require further investigation (25).
Continued research into these factors is essential for developing targeted interventions aimed at reducing the global burden of diabetes.
Diagnosis of Diabetes
Diabetes may manifest in different ways, but recognizing its symptoms is crucial for early detection and management. While type 1 diabetes often presents sudden symptoms, other types may develop more gradually, making them less noticeable. To aid in early identification, the American Diabetes Association (ADA) has established screening guidelines. Here’s who should consider screening for diabetes:
- Age Consideration: Those over the age of 35 are encouraged to undergo an initial blood sugar screening. If the results are within the normal range, subsequent screenings should be conducted every three years (26)
- Body Mass Index (BMI) Consideration: Individuals with a BMI over 25 should consider screening, especially if they have additional risk factors. These factors include abnormal cholesterol levels, high blood pressure, a history of polycystic ovary syndrome or heart disease, a sedentary lifestyle, and a family history of diabetes (27).
- Prediabetes Diagnosis: Individuals diagnosed with prediabetes should undergo annual testing to monitor their condition closely (26)
- Gestational Diabetes History: Women who have experienced gestational diabetes during pregnancy should undergo screening for diabetes every three years (28).
- HIV Diagnosis: Individuals living with HIV should also undergo regular testing for diabetes (29).
Regular screening is vital for early detection and timely intervention, which might significantly improve outcomes and quality of life for individuals with diabetes. By staying informed and proactive, we may better manage this condition and minimize its impact on our health.
Remember, if you have any concerns about diabetes or your risk factors, consult with a healthcare professional for personalized guidance and support. Your health is worth prioritizing!
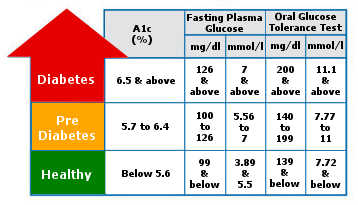
Tests for type 1 and type 2 diabetes and prediabetes
It’s essential to diagnose diabetes early to manage it effectively and prevent complications. Here’s a breakdown of the tests used to diagnose type 1 and type 2 diabetes, as well as prediabetes.
- A1C Test: One of the primary tests for diagnosing diabetes is the A1C test. This blood test measures your average blood sugar level over the past 2 to 3 months, without requiring fasting. It assesses the percentage of blood sugar attached to hemoglobin, a protein in red blood cells that carries oxygen.
- Fasting Blood Sugar Test: The fasting blood sugar test involves taking a blood sample after an overnight fast. (30)
- Random Blood Sugar Test: Another diagnostic tool is the random blood sugar test, which might be done at any time regardless of fasting (31).
- Glucose Tolerance Test: During the glucose tolerance test, you fast overnight before having your fasting blood sugar level measured. Then, you consume a sugary drink, and your blood sugar levels are monitored over the next two hours (32).
- Gestational Diabetes Screening: Pregnant individuals are also screened for gestational diabetes, a type of diabetes that occurs during pregnancy. High-risk individuals may undergo testing during the first prenatal visit, while those at average risk are usually screened during the second trimester (33).
- Additional Tests: For individuals suspected of having type 1 diabetes, urine tests may be conducted to detect the presence of ketones, which are byproducts produced when the body uses muscle and fat for energy. Additionally, autoantibody tests may be performed to identify destructive immune system cells associated with type 1 diabetes (34).
Early diagnosis of diabetes through these tests enables healthcare providers to initiate appropriate treatment and lifestyle modifications, promoting better management of the condition and reducing the risk of complications. If you have concerns about diabetes or your risk factors, consult your healthcare provider for personalized guidance and support.
Treatment of Diabetes
Diabetes treatment varies depending on the type of diabetes one has. It typically involves a combination of blood sugar monitoring, medication (such as insulin or oral drugs), lifestyle adjustments, and sometimes surgical interventions.
Type 1 Diabetes
Diabetes, particularly Type 1, requires careful management to maintain optimal health. Here are key strategies for managing Type 1 Diabetes:
- Insulin Therapy: Individuals with type 1 diabetes rely on insulin injections or insulin pumps to manage their blood sugar levels.
- Blood Sugar Monitoring: Regular blood sugar checks and carbohydrate counting are crucial for maintaining control (35).
- Transplant Options: Pancreas or islet cell transplants may be considered for some individuals (36).
Individuals considering these options should weigh the potential benefits against the risks and consult with healthcare providers.
Type 2 Diabetes
When it comes to managing Type 2 diabetes, a multifaceted approach is key. This involves making significant lifestyle adjustments, adhering to medication regimens, and closely monitoring blood sugar levels.
- Lifestyle Changes: Managing type 2 diabetes often involves adopting a healthy diet, maintaining a healthy weight, and engaging in regular physical activity (37).
- Medication: Oral diabetes drugs, insulin, or a combination of both may be prescribed (38).
- Monitoring: Regular blood sugar monitoring is essential, although the frequency varies based on treatment plans (39).
- Blood Sugar Monitoring: Depending on the treatment plan, individuals may need to check their blood sugar levels multiple times a day. Continuous glucose monitors are becoming more popular, offering real-time insights into blood sugar trends (40).
- A1C Testing: A1C tests, conducted every 2 to 3 months, provide an overview of average blood sugar levels. These tests help gauge the effectiveness of the treatment plan (41).
- Insulin Therapy: Type 1 diabetes requires insulin for survival, and some individuals with type 2 diabetes may also need insulin therapy. Various types of insulin are available, administered through injections, insulin pens, or insulin pumps (42).
- Continuous Glucose Monitors and Insulin Pumps: Continuous glucose monitors measure blood sugar levels continuously, offering valuable data for insulin dosing. Insulin pumps deliver insulin in a controlled manner, mimicking the function of a healthy pancreas (43).
- Other Medications: Besides insulin, other oral or injected drugs may be prescribed to manage blood sugar levels. These medications work in different ways, such as increasing insulin production or improving insulin sensitivity (38).
- Transplantation and Surgical Options: Pancreas transplants or islet transplants may be considered for select individuals with type 1 diabetes. Bariatric surgery may benefit some individuals with type 2 diabetes, especially those who are obese. However, its long-term effects on diabetes control are still under study (44).
While transplantation and surgery offer potential benefits, they also carry significant risks and may not be suitable for everyone.
Managing diabetes requires a multifaceted approach, including medication, lifestyle modifications, and sometimes surgical interventions. By working closely with healthcare providers and adopting a proactive approach to self-care, individuals with diabetes may effectively manage their condition and lead fulfilling lives.
Treatment For Gestational Diabetes
When it comes to gestational diabetes, maintaining optimal blood sugar levels is crucial for both your health and your baby’s well-being during pregnancy. By adopting a balanced diet and engaging in regular exercise, you lay a solid foundation for effective management (45). Additionally, your healthcare provider may recommend monitoring your blood sugar levels closely. In certain situations, insulin therapy or oral medications might also be prescribed to maintain blood sugar within a healthy range.
During labor, your healthcare provider will continuously monitor your blood sugar levels. Elevated blood sugar levels might trigger an excessive release of insulin in your baby, potentially resulting in low blood sugar levels shortly after birth.
Addressing Prediabetes
Prediabetes treatment primarily revolves around embracing healthier lifestyle choices. These lifestyle adjustments play a pivotal role in bringing your blood sugar levels back to normal or preventing them from escalating towards the thresholds characteristic of type 2 diabetes. Maintaining a healthy weight through regular exercise and nutritious eating habits is key. Engaging in physical activity for at least 150 minutes per week and aiming to shed body weight may significantly lower the risk of developing type 2 diabetes (46)
In some cases, medications such as metformin, statins, or medications to manage high blood pressure may be considered, especially for individuals with prediabetes who also have concurrent conditions like heart disease. However, lifestyle modifications remain the cornerstone of prediabetes management.
Prevention of Diabetes
While type 1 diabetes cannot be prevented, making healthy lifestyle choices may significantly reduce the risk of developing prediabetes, type 2 diabetes, and gestational diabetes:
- Maintain a Healthy Weight: Shedding excess pounds, even a modest 7% of your body weight, might significantly lower the risk of diabetes. For instance, if you weigh 200 pounds (90.7 kilograms), losing 14 pounds (6.4 kilograms) may decrease your diabetes risk (47). However, it’s crucial not to attempt weight loss during pregnancy. Consult your healthcare provider to determine a healthy weight gain range for your pregnancy (48).
- Choose Nutritious Foods: Opt for foods that are low in fat and calories while being high in fiber. Prioritize a diet rich in fruits, vegetables, and whole grains. Variety in your food choices may help keep your meals interesting and satisfying (49).
- Stay Active: Aim for at least 30 minutes of moderate aerobic activity most days of the week. Alternatively, strive for a total of 150 minutes of moderate aerobic activity weekly. Activities like brisk walking may easily fit into your daily routine. If finding time for a single long workout is challenging, break it down into smaller sessions spread throughout the day (50).
- Adopt Sustainable Habits: Focus on making long-term adjustments to your eating and exercise routines to keep your weight within a healthy range. Recognize the numerous benefits of weight loss, such as a healthier heart, increased energy levels, and enhanced self-esteem (51).
- Consider Medical Options: In some cases, medications may be recommended. Oral diabetes medications like metformin (sold under various brand names such as Glumetza, Fortamet, etc.) could help lower the risk of developing type 2 diabetes (52).
Nonetheless, prioritizing healthy lifestyle choices remains paramount. If you have prediabetes, ensure you undergo blood sugar checks at least annually to monitor for any progression to type 2 diabetes.
Conclusion
In conclusion, diabetes is a complex but manageable condition that affects millions of people worldwide. By adopting healthy lifestyle habits, such as regular exercise, a balanced diet, monitoring blood sugar levels, and following prescribed treatment plans, individuals with diabetes might effectively manage their condition. Additionally, with continued research and advancements in medical technology, there is hope for improved treatments and ultimately, a better quality of life for those living with diabetes. Remember, knowledge is power when it comes to managing diabetes, and with the right tools and support, individuals may lead fulfilling lives despite their diagnosis.