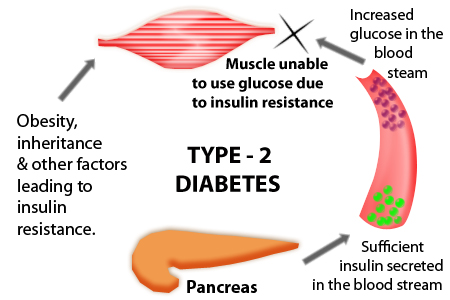
Type 2 diabetes is a complex multifactorial disease whose exact origins have not been understood. However, lots of research has been done and more will be performed in the coming years. Some of this research has dealt with the complications, which include renal, ocular and neurological damage. This had led to serious economic cost and detrimental effects on millions of lives. This is the result of the current epidemic that includes type 2 diabetes and other diseases such as dyslipidemias and obesity. It is estimated that about one-quarter of patients with diabetes have not been diagnosed with diabetes. This could be explained by the progressive nature of type 2 diabetes. Additionally, during early stages glucose levels are not high enough to produces signs and symptoms. Only through adequate screening leading to an early diagnosis can the damage caused by type 2 diabetes be prevented.
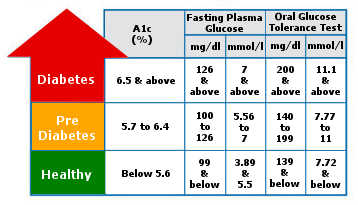
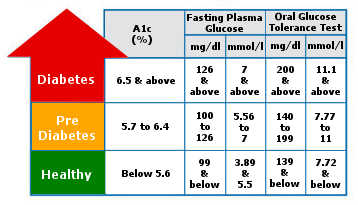
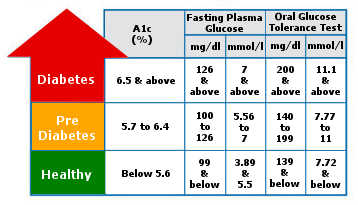
Table of Contents
Type 2 Diabetes Diagnosis
The diagnosis of type 2 diabetes revolves around the proper screening of patients, evaluation of their clinical manifestations and the adequate use of type 2 diabetes tests. Additionally, the patients must be evaluated for the possible complications resulting from type 2 diabetes.
The first step in type 2 diabetes diagnosis is the screening for patients with an increased risk or patients with asymptomatic diabetes. Usually, this is based on risk factors found in the epidemiological data acquired from research. The physician must remember to distinguish adult and pediatric populations as the current guidelines have different risk factor criteria associated with each population. This an important fact because it also reminds the physician that regardless that type 2 diabetes is commonly associated with patients over 45 years old, there must be a regular evaluation of at-risk pediatric patients.
Patients normally can live for a long period of their lives without being aware of their risk or diabetic condition. However, as patient ages, the symptoms and signs of type 2 diabetes and complications may appear the need for type 2 diabetes test becomes more obvious. Particularly at age 45, the risk of type 2 diabetes significantly increases. Therefore, all patients starting from this age and on must be subjected to a type 2 diabetes test, which includes the fasting plasma glucose, the glucose tolerance test or the glycosylated hemoglobin test. If the results turn out to be normal the patient must perform the same test minimally in a 3-year interval. However, there are additional considerations to be taken in the screening in adults.
As seen in the Standards of Care of Diabetes, the increased weight, one of the major risk factors for type 2 diabetes, has been taken into consideration. This guideline indicates that patients who are overweight (defined as a body mass index greater than 25 kg/m2 or 23 kg/m2in Asian Americans) with additional risk factors should be considered for type 2 diabetes testing. This means all adult patients, even those without symptoms, should be screened if they are identified as overweight and present at least one risk factor. These risk factors can be grouped into genetic risk factors, lifestyle risk factors, and associated clinical conditions.
In the guideline, only the only genetic risk factor considered is the presence of a first-degree relative with diabetes and the only lifestyle risk factor is physical inactivity. However, race and ethnicity are also considered. Among the group with high risk are native Americans, African Americans, Asian Americans, and Pacific Islanders. It has not been determined if this risk factor is a genetic or cultural one, but it is most likely the results of both.
The associated clinical conditions are hypertension, dyslipidemias, macrosomia babies, gestational diabetes, polycystic ovary syndrome, and other conditions associated with insulin resistance.
The Standards of Care has also established similar guidelines for pediatric patients but has certain differences. The screening type 2 diabetes test for pediatric populations does not include the glycosylated hemoglobin. Additionally, the previous practical definition of the risk factors in pediatrics differ. For example, overweight children are defined by having a body mass index superior to the 85th percentile for children’s the same age and sex. Another way of identifying overweight pediatric patients is comparing weight for height (if this is greater than the 85th percentile or weight higher than 120% than the ideal weight for height). Additionally, screening in pediatrics is recommended when the patients are identified as overweight and present at least 2 risk factors starting from the onset of puberty or when the patient turn 10 years old.
Genetic risk factors in pediatric patients include a family history of type 2 diabetes in a first or second-degree relative. Race or ethnicity is a risk factor in a similar manner to the adult population. Also, signs of insulin resistance and other conditions associated with acanthosis nigricans, dyslipidemias, and many others, are also similar to the adult population. However, small-for-gestational-age birth weight is also a risk factor associated with insulin resistance that must be considered as a risk factor. Other risk factors in the pediatric population include the maternal history of diabetes or gestational diabetes mellitus during pregnancy (of the specific patient).
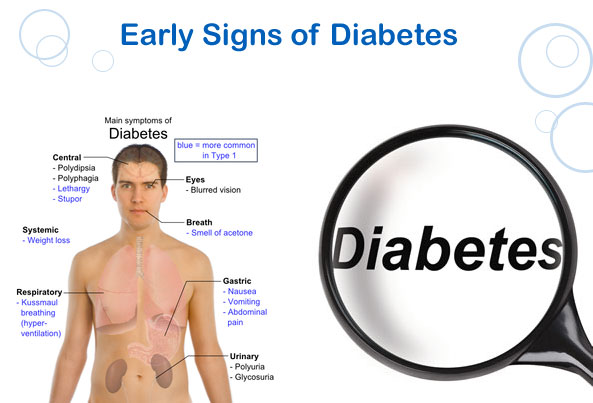
Apart from risk factors, clinical manifestations might indicate type 2 diabetes testing, but in this case to confirm the diagnosis of type 2 diabetes. The clinical manifestation can be the result of direct effects of hyperglycemic state induced by type 2 diabetes or complications of the disease. The direct effects can be described as the initial manifestations. Among these initial manifestations are the classic symptoms of type 2 diabetes along with other signs and symptoms associated with type 2 diabetes.
The classic symptoms of type 2 diabetes include polyphagia, polyuria, polydipsia. The three signs are induced by the interaction of the hyperglycemic state and the regular physiological process. Additionally, patients might present signs and symptoms such as blurry vision, frequent infections, fatigue, and acanthosis nigricans.
Type 2 diabetes might present other manifestations resulting from an acute complication called a nonketoic hyperosmolar state. Other clinical manifestations associated with type 2 diabetes are those resulting from chronic complications from type 2 diabetes. These complications are grouped according to the type of vascular damage that mediates each, either as damage to the microvasculature or damage to the macrovasculature. Microvasculature damage includes lesions to the kidneys, retina, and nerves, while macrovasculature includes damages to the heart, large vessels, and cerebrovascular systems.
The physician will use type 2 diabetes test as a screening tool after studying the patient’s risk factors or as a confirmation test upon exploring the clinical manifestations. It is the result of these tests that will either identify the patients as having regular results, prediabetes or diabetic. There are four tests to evaluate patients, random glucose test, the fasting plasma glucose test, the glucose tolerance test or the glycosylated hemoglobin test.
The first and last of the mentioned type 2 diabetes test do not require fasting and involve simply the extraction of a blood sample. However, in the random glucose test, the quantity of the concentration of glucose is measured in the sample. On the other hand, the glycosylated hemoglobin test measures the combination of hemoglobin A and glucose. This means that the glycosylated hemoglobin test provides a retrospective measurement of plasma glucose levels. It must be noted that the conditions in which there is an increased turnover of red blood cells or in pediatric populations, the physician should perform other tests additional to the glycosylated hemoglobin test.
The other two, fasting glucose test and the glucose tolerance test do require fasting for a period of at least 8 hours. However, in the first, a single measurement is taken. While in the glucose tolerance test after the initial fasting glucose is measured, the patient is given 75 grams of glucose and blood is tested every 30 minutes for two hours.
If the results of the type 2 diabetes test are irregular, these can identify prediabetes or diabetes in a patient.
The any of following results identifies prediabetes in patients
- Glycosylated hemoglobin ranging from 5.7 to 6.4%
- Fasting plasma glucose ranging from 100 to 125 mg per deciliter
- 2-hour plasma glucose after an oral glucose test ranging from 140 to 199 mg per deciliter
The any of following results identify a patient as diabetic
- Glycosylated hemoglobin test equal to or greater than 6.5%
- Fasting plasma glucose equal to or greater than 126 mg per deciliter
- 2-hour plasma glucose after an oral glucose test equal to or greater than 200 mg per deciliter
- Random plasma glucose equal to or greater than 200 mg per deciliter in patients with classic symptoms of hyperglycemia or a hyperglycemic crisis
Some physician also orders a laboratory test to determine insulin levels in patients. This test consists of the evaluation of insulin levels through an ac-peptide test or fasting insulin test. The c-peptide test is useful for evaluating cases in which type 1 diabetes must be discarded. Usually, type 1 diabetes has no production of insulin while type 2 does (however levels can be higher, normal or lower in type 2 diabetes). While the fasting insulin test is said to be able to provide information on insulin insensitivity of the patient.
Additionally, there are other type 2 diabetes tests that are oriented towards measuring insulin as well as commonly used for research papers. It has been observed that these tests could allow for earlier detection of insulin resistance or patients at risk of developing type 2 diabetes. These tests include the glucose tolerance/insulin response test and the Hyperinsulinemic-euglycemic clamp test.
The glucose/insulin response test is similar to a glucose challenge test but instead, both insulin and glucose are measured across the study. These will result in an insulin response pattern which can be used to evaluate the risk of the patient developing resistance or if the patient already presents resistance.
The Hyperinsulinemic-euglycemic clamp test has been considered the golden standard to evaluate insulin insensitivity. The test consists of the infusion of insulin and glucose to determine the amount of glucose need to prevent hypoglycemia in patients with increased insulin levels.
It must be noted that these tests are not commonly used in a clinical environment but perhaps there could be benefits in the clinical application of these. However, it could add unnecessary cost to patient evaluation if they are not properly researched. More research is needed to determine their utility and to compare their benefit compared to classical glucose test. Additionally, several models (the homeostatic model assessment and the quantitative insulin sensitivity check index) have been created to measure insulin insensitivity indirectly. They use fasting glucose and insulin levels to calculate the insulin insensitivity and have shown good correlation with glucose clamp studies. However, similarly to the direct insulin test, the clinical utility of these models need to be established.
The physician can also order additional tests to detect comorbidities associated or caused by type 2 diabetes. These include fasting lipid profile (total, LDL, and HDL cholesterol and triglycerides), liver function test, spot urinary albumin-to-creatinine ratio, serum creatinine ratio, and estimated glomerular filtration rate, and thyroid-stimulating hormone in certain patients (patients with dyslipidemia or women older than 50 years old).
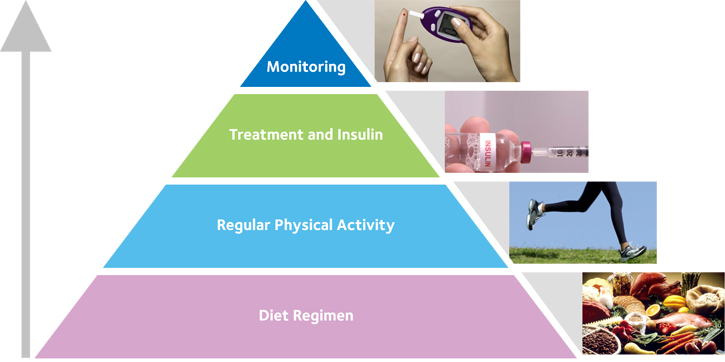
Once the physician receives these results the type 2 diabetes test the other half of patient care begins, management. The physician will establish a plan based on the needs and possible risk of the patient to lower and maintain adequate sugar levels. However, the physician must also evaluate the damage that has occurred already or might develop. That’s why the diagnosis of type 2 diabetes is not done with the diagnosis of the disease itself, but also the required the diagnosis of the chronic complications which have been reviewed briefly. To do so, the physician will examine the patient and if needed refer him to the specialist. Guidelines include the following referrals as part of the initial management, annual dilated eye exam, dental examination, and nutritional specialist evaluation.
However, the success of the management in a patient diagnosed with type 2 diabetes will depend on how early its diagnosis was made. Only through screening, a physician will be able to indicate the necessary test to diagnose type 2 diabetes and prevent the cost and life treating complications arising from this global epidemic. Diagnosis is known to be the most important thing in treating this chronic disease and keeping the patient healthy and functioning. If this is done wrong, the whole treatment may be wrongfully chosen and this can result in various complications, starting from a mild one to very serious ones, even the death of the patient.