Sleep apnea affects a significant portion of adults globally. Studies suggest that approximately 10 to 15% of adults worldwide experience this condition. In the United States, research indicates that about 26% of individuals aged 30 to 70 years old are affected by sleep apnea (1) .
Table of Contents
What is Sleep Apnea?
Sleep apnea is a significant sleep disorder characterized by irregularities in breathing during sleep. These irregularities may lead to various complications if left untreated, ranging from disruptive snoring and daytime fatigue to more severe health issues such as cardiovascular problems and hypertension (2).
It’s important to distinguish sleep apnea from regular snoring (3). While primary snoring may stem from factors like nasal or throat issues, sleep posture, excess weight, aging, or the use of alcohol and sedatives, sleep apnea involves recurrent disruptions in breathing patterns during sleep.
Although sleep apnea itself isn’t typically considered fatal, studies indicate that individuals with untreated sleep apnea face a higher risk of sudden death compared to those without the condition (4) . This elevated risk is largely attributed to the disorder’s association with serious health conditions such as hypertension, cardiovascular diseases, strokes, and diabetes. Therefore, timely diagnosis and management of sleep apnea are crucial for mitigating potential health risks.
Type of Sleep Apnea
Sleep apnea manifests in several forms, with the primary ones being:
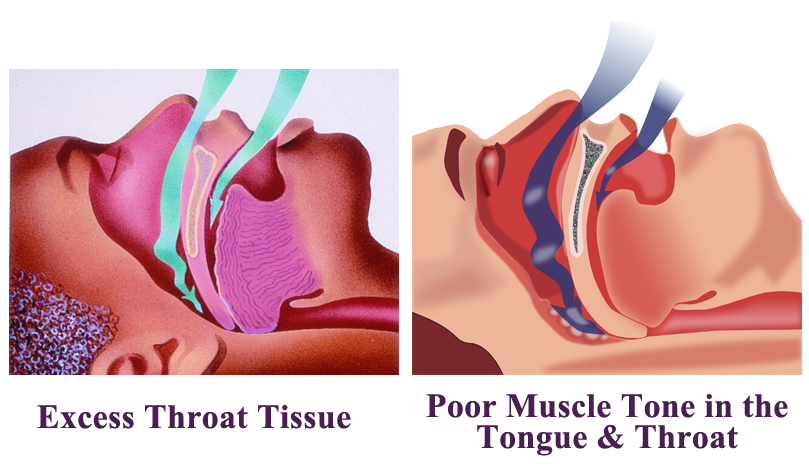
- Obstructive Sleep Apnea (OSA): This form is the most prevalent, characterized throat muscles relaxing during sleep, leading to the obstruction of airflow into the lungs (5).
- Central Sleep Apnea (CSA): In this type, the brain fails to transmit proper signals to the muscles responsible for regulating breathing during sleep (6).
- Treatment-Emergent Central Sleep Apnea: Also recognized as complex sleep apnea, this variant occurs when a person initially diagnosed with OSA, through a sleep study, transitions to CSA upon receiving therapy for OSA (7).
Effective treatment not only alleviates symptoms but also helps mitigate the risk of developing heart problems and other associated complications.
Severity Levels of Sleep Apnea
The severity of sleep apnea is assessed through sleep testing, which monitors the frequency of these breathing interruptions per hour. Based on the results, doctors may diagnose the condition and classify its severity into three main categories (8):
- Mild Sleep Apnea: Individuals with mild sleep apnea experience an average of 5 to 15 breathing interruptions per hour during sleep. While this level of severity may not pose immediate health risks, it still requires attention and management to prevent potential complications.
- Moderate Sleep Apnea: Moderate sleep apnea is diagnosed when a person experiences between 15 and 39 breathing interruptions per hour during sleep. At this level, the condition may start to significantly impact sleep quality and overall well-being, warranting intervention and treatment to mitigate risks and improve sleep patterns.
- Severe Sleep Apnea: Severe sleep apnea is characterized by more than 30 breathing interruptions per hour during sleep. At this level of severity, the condition poses significant health risks, including cardiovascular complications, daytime fatigue, and cognitive impairment.
Understanding the severity of sleep apnea is crucial for timely intervention and management. If you suspect you or someone you know may have sleep apnea, consulting a healthcare professional for evaluation and appropriate testing is recommended.
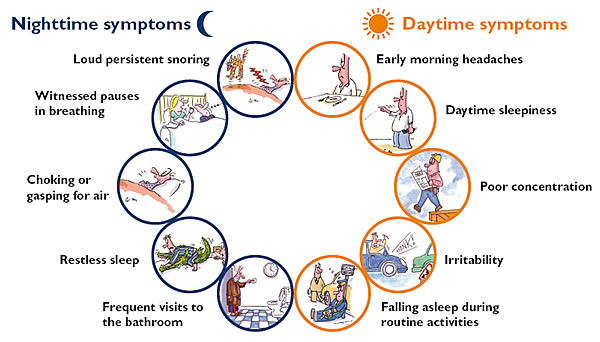
Symptoms of Sleep Apnea
Sleep apnea may significantly impact daily life and overall health if left untreated. While it may go unnoticed by the affected individual, often, it’s a partner or family member who first notices the signs. Recognizing these symptoms early is crucial for timely intervention and management:
- Snoring: Persistent, loud snoring is one of the hallmark symptoms of sleep apnea. It occurs due to the partial obstruction of the airway during sleep (5).
- Restlessness or Frequent Awakening: Disrupted sleep patterns characterized by restlessness or frequent awakenings during the night are common symptoms of sleep apnea (9).
- Gasping or Choking Episodes: Sudden awakenings accompanied by gasping or choking sensations may occur as the body tries to restore normal breathing patterns (10).
- Dry Mouth or Sore Throat: Waking up with a dry mouth or sore throat may be indicative of breathing difficulties during sleep, such as those experienced in sleep apnea (11).
- Mood Changes: Depression or anxiety may result from chronic sleep disruption caused by sleep apnea (12).
- Trouble Concentrating or Forgetfulness: Cognitive symptoms like trouble concentrating, forgetfulness, or irritability are often reported by individuals with sleep apnea (13).
- Night Sweats: Excessive sweating during sleep, especially when not related to room temperature or bedding, may be a symptom of sleep apnea (14).
- Frequent Nighttime Urination: The need to urinate frequently during the night, known as nocturia, may disrupt sleep and may be linked to sleep apnea (15).
- Sexual Dysfunction: Some individuals with sleep apnea may experience sexual dysfunction, possibly due to the effects of chronic sleep deprivation on hormone levels and overall health (16).
Symptoms in Children
Symptoms of sleep apnea in children may differ from those in adults and may include sluggishness, hyperactivity, poor academic performance, difficulty swallowing, mouth breathing during the day, unusual sleeping positions, excessive sweating at night, heartburn, and bedwetting (17).
If you or someone you know experiences any of these symptoms, especially if they persist over time, it’s essential to consult a healthcare professional for proper evaluation and management.
Causes and Risk Factors of Sleep Apnea
Sleep apnea is a condition that may affect people of any age, including children. However, certain factors may elevate the risk of developing this disorder.
Obstructive Sleep Apnea (OSA)
Obstructive sleep apnea is influenced by various factors, including:
- Weight: Excessive weight, particularly obesity, is a significant risk factor for OSA. Accumulation of fat around the upper airway may lead to breathing obstructions during sleep (18).
- Airway Narrowness: Inherited traits such as a naturally narrow throat or enlarged tonsils/adenoids, especially in children, may contribute to airway blockages (19).
- Neck Circumference: Individuals with thicker necks may have narrower airways, predisposing them to OSA (20).
- Sex: Individuals assigned male at birth (AMAB) are at a higher risk, being 2 to 3 times more likely to develop sleep apnea compared to those assigned a different sex. However, overweight women or those who have undergone menopause also face increased risk (21).
- Age: Sleep apnea is more prevalent among older adults (22).
- Smoking: Smokers have a threefold higher likelihood of developing obstructive sleep apnea due to increased inflammation and fluid retention in the upper airway (23).
- Family History: Having relatives with sleep apnea might elevate individual susceptibility (24).
- Nasal Congestion: Difficulty breathing through the nose, whether due to structural issues or allergies, heightens the risk of OSA (25).
- Medical Conditions: Certain health conditions like congestive heart failure, hypertension, and type 2 diabetes are associated with an increased risk of OSA (26).
Additionally, disorders such as polycystic ovary syndrome, hormonal imbalances, prior stroke, and chronic lung diseases like asthma may also elevate susceptibility (27).
Central Sleep Apnea (CSA)
Risk factors for central sleep apnea include:
- Heart Disorders: Congestive heart failure is a significant risk factor (28).
- Age: Middle-aged and older individuals are at a higher risk (29).
- Sex: Central sleep apnea is more prevalent in biological males (AMAB) (30).
- Stroke: Individuals who have experienced a stroke are at an elevated risk of developing central sleep apnea (31).
- Narcotic Pain Medications: The use of opioid medications, especially long-acting ones like methadone, may increase the risk of CSA (32).
Understanding these causes and risk factors is crucial for early detection and effective management of sleep apnea.
Diagnosis of Sleep Apnea
Identifying sleep apnea typically starts with a thorough evaluation of your symptoms and sleep patterns, which may be aided by input from someone who shares your sleeping space. Your healthcare provider may then refer you to a specialized sleep disorder center for further assessment.
The evaluation process often entails overnight monitoring of your vital signs and bodily functions during sleep, conducted at a designated sleep center. Alternatively, you may be offered the option of conducting tests at home.
Diagnostic tests for sleep apnea may include:
- Nocturnal polysomnography: This comprehensive test involves monitoring various physiological parameters such as heart rate, brain activity, breathing patterns, and blood oxygen levels while you sleep (33).
- Home sleep tests: These simplified tests, provided by your healthcare provider, allow for monitoring of vital signs like heart rate, blood oxygen levels, airflow, and breathing patterns from the comfort of your own home. However, polysomnography in a clinical setting is often preferred, especially if central sleep apnea is suspected (34).
In cases where initial test results are inconclusive, further diagnostic testing may be necessary. It’s important to note that portable monitoring devices may not always detect sleep apnea accurately, which is why polysomnography remains a preferred option for definitive diagnosis.
For individuals diagnosed with obstructive sleep apnea, additional referrals may be made to specialists such as ear, nose, and throat (ENT) doctors to investigate potential blockages in the upper airway . Furthermore, consultations with cardiologists or neurologists may be required to explore underlying causes of central sleep apnea.
Treatment of Sleep Apnea
Various strategies may effectively reduce or alleviate sleep apnea symptoms. Your doctor will tailor the treatment plan according to the severity of your condition. For milder cases, lifestyle modifications may suffice, such as weight loss, quitting smoking, or addressing nasal allergies if present.
In cases where symptoms persist or worsen, especially in moderate to severe sleep apnea, alternative treatments become necessary.
Sleep Apnea Machines (CPAP/BPAP/ASV/Auto-PAP)
Several devices are available to manage sleep apnea, all utilizing masks worn over the face during sleep to deliver air into the airways. If discomfort arises from the mask, discussing alternatives with your doctor is advisable.
- Continuous Positive Airway Pressure (CPAP): This common device maintains open upper airway passages by delivering air through a mask covering the nose and mouth (35).
- Bilevel Positive Airway Pressure (BPAP or BiPAP): Unlike CPAP, BPAP adjusts air pressure, providing higher force during inhalation, which may suit some individuals better (36).
- Adaptive Servo-Ventilation (ASV): ASV devices learn individual breathing patterns and adjust air pressure levels accordingly, proving particularly effective for complex sleep apnea treatment (37).
- Auto-Positive Airway Pressure Machine (Auto-PAP or APAP): This device automatically adapts air pressure levels during sleep, accommodating changes in breathing patterns (38).
Oral Appliances
Alternatively, oral appliances like sleep mouth guards or tongue-retaining devices may help keep the throat open (39). Though less effective than positive airway pressure machines, they may be more user-friendly. Consulting a dentist may aid in finding the suitable appliance.
Supplemental Oxygen
Central sleep apnea may necessitate supplemental oxygen during sleep. Various forms of oxygen delivery systems exist to support breathing (40) .
Medications
While no specific drugs are FDA-approved for sleep apnea, physicians may prescribe sleep aids or medications to aid breathing, especially for central sleep apnea (41) .
Surgical Options
When other treatments prove ineffective, surgery might be considered, typically after a three-month trial of alternative therapies or in the presence of structural jaw issues. Surgical procedures may include:
- Nerve Stimulation: Involves implanting a device to stimulate the tongue-controlling nerve, preventing airway blockage (42).
- Jaw Repositioning: Adjusting the jaw position to create more space behind the tongue and palate (43).
- Tissue Shrinkage: Noninvasive procedure using radiofrequency waves to reduce tissue size in the mouth and throat (44).
- Tissue Removal: Surgical removal of excess tissue in the mouth and throat, including tonsils and adenoids (45).
- Other Surgical Interventions: Such as removing large tonsils or adenoids or weight loss surgery, which may aid in reducing snoring and managing sleep apnea.
From lifestyle modifications to surgical interventions, various options exist to alleviate symptoms and improve quality of life for individuals with sleep apnea. It is essential to consult with healthcare professionals to determine the most appropriate treatment plan based on the severity of the condition and underlying health factors.
Prevention of Sleep Apnea
Sleep apnea may significantly impact one’s quality of life and overall health. Fortunately, there are several lifestyle modifications and habits that might help manage and even prevent this condition.
- Regular physical activity plays a vital role in controlling weight and improving sleep quality. Aim for at least 30 minutes of exercise on most days of the week to reap the benefits.
- Maintaining a healthy diet. Research indicates that adopting a Mediterranean diet, rich in fruits, vegetables, and whole grains, may reduce the frequency of apnea episodes, regardless of weight loss.
- Consulting with a healthcare provider for personalized dietary guidance is recommended to achieve and maintain a healthy weight.
- Practicing good sleep hygiene promotes restful sleep. Consistency in sleep schedule, a conducive sleep environment (dark, cool, and quiet), and minimizing electronic device use before bedtime may aid in better sleep quality.
- Sleeping on your side may also prevent airway collapse, as sleeping on your back increases the likelihood of obstruction. While sleeping on your stomach may reduce snoring, it may strain the back and neck.
- Elevating the head during sleep may help keep air passages open. Utilizing a wedge pillow or adjustable bed may assist in maintaining proper positioning.
- Avoiding substances that disrupt sleep, such as cigarettes, alcohol, and sedatives, is essential for managing sleep apnea symptoms effectively.
- Sticking to prescribed treatments, such as positive airway pressure (PAP) therapy, is crucial for optimal outcomes. Communicating any difficulties with treatment to healthcare providers ensures timely adjustments and support.
Note: Driving with untreated sleep apnea poses risks of accidents (46, 47) . It’s advisable to refrain from driving until treatment effectiveness is confirmed. Having a companion in the vehicle or seeking evaluation from a driver rehabilitation specialist or occupational therapist may aid in assessing driving safety.
By implementing these strategies and seeking appropriate medical guidance, individuals may effectively manage and reduce the impact of sleep apnea on their daily lives.
Conclusion
The impact of sleep apnea extends beyond just disturbed sleep, leading to various health complications such as hypertension, cardiovascular diseases, and cognitive impairments. However, with proper diagnosis and treatment, individuals suffering from sleep apnea may significantly improve their quality of life and reduce the risk of associated health problems.
Addressing sleep apnea requires a multidisciplinary approach involving healthcare providers, patients, and their families. By working together, we might alleviate the burden of sleep apnea and help individuals achieve restful and rejuvenating sleep, leading to better overall health and well-being.